Introduction
Interventional pulmonology is a growing subspecialty in pulmonary medicine with remarkable advancements in recent years having been made in diagnostic and therapeutic innovations. Different procedures require different anesthetic considerations based on the complexity of the procedure performed and underlying patient conditions; these range from conscious sedation to general anesthesia. Here We present a case series where we discuss the various methods used for securing the airway as well as the pharmacologic considerations, ventilation modes, and potential complications relevant to the different interventional bronchoscopic procedures.
Case report
Case 1
58/F Diagnosed as left thigh sarcoma with lung secondaries presented with dry cough and exertional dyspnea for 1 yr. k/c/o SHTN on medication and no other comorbid conditions. CT thorax plain soft tissue lesion 5×3 cm noted in the subcarinal region causing mass effect and narrowing of left main bronchus. TIVA with moderate sedation with nasopharyngeal airway and maintaining spontaneous ventilation all through the procedure. Tracheal Y stenting through flexible bronchoscope under fluoroscopy guidance. Post procedure patient conscious , stable and shifted to recovery .
Case 2
48/F diagnosed as case of tracheal stenosis (?post intubation ) H/o pulmonary edema leading to collapse of the patient- intubated and resuscitated and on ventilator for 4 days extubated after recovery and discharged 3 months ago.K/c/o NSTEMI ,SHTN,DM,CKD on treatment ,patient presented with noisy breathing ,cough with expectoration and breathlessness on exertion for 4 days.Cardiology and nephrology fitness for surgery was obtained
Spirometry – Fixed intrathoracic airway obstruction with reduction in both inspiratory and expiratory flow.
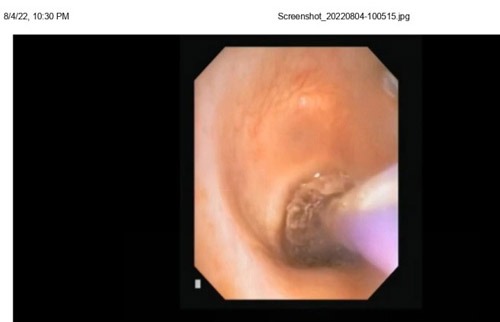
CT thorax plain –Narrowing of proximal trachea noted for a length of 1 cm with AP and transverse diameter 5 and 7 mm respectively in the level of T1 vertebra. Moderate sedation with BASKA mask and spontaneous assisted ventilation. Controlled Radial Expansion (CRE) balloon dilatation at the stenosis site was performed for around 30 seconds for 3 times. Post procedure patient conscious , stable and shifted to recovery .
Case 3
70/M Left hilar mass with left upper lobe collapse (? Bronchogenic carcinoma )No known comorbid conditions Presented with breathlessness, cough with expectoration,loss of weight and appettite for 6 months .CECT Thorax Left hilar mass causing left lung collapse Few soft tissue density nodules in the medial basal ,anterior basal and posterior basal segment of right lower lobe . General anaesthesia with short acting mucle relaxant.Rigid bronchoscopy guided cryo biopsy done. Post procedure patient conscious , stable and shifted to recovery .
Case 4
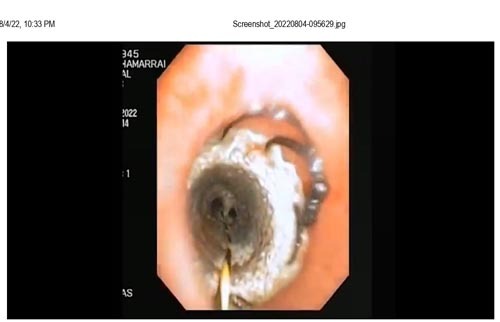
36/M Right sided pyopneumothorax (tubercular) with bronchoplueral fistula with right ICD insitu .K/c/o SHTN and DM under medication with past history of covid. presented with cough with expectoration for 3 months. h/o fever intermittent with evening rise in temperature no chills and rigor patient was on antitubercular drug.CT thorax plain : Right moderate hydropneumothorax with passive right lung collapse with icd insitu ,possibility of peripheral bronchopleural fistula ( air component is more than that of fluid component with ICD insitu ) Moderate to deep sedation with BASKA mask and spontaneous ventilation. Flexible bronchoscopy guided closure of fistula done with spigot and endocryl. . Post procedure patient conscious , stable and shifted to recovery
Conclusion
Anaesthesia for interventional bronchoscopy procedures carry increased risk because most of the patients will have poor lung funtion and associated comorbid conditions A thorough evaluation of individual comorbidities, risk factors, and technical aspects associated with each procedure is necessary. Given that interventional pulmonologists and the anesthesia team share the working field, constant communication between specialists is fundamental
Key words
bronchoscopy procedures , BASKA mask, TIVA