| S. No. | Faculty Name | Designation | Department |
| 1 | Dr. T.Bharath Kumar | Professor and Head | Paediatrics |
| 2 | Dr. Arul Kumaran. A | Professor | Paediatrics |
| 3 | Dr. Kanimozhi. T | Professor | Paediatrics |
| 4 | Dr. Preethi. T | Professor | Paediatrics |
| 5 | Dr. Pradeep. S | Associate Professor | Paediatrics |
| 6 | Dr. Arun Kumaar | Assistant Professor | Paediatrics |
| 7 | Dr. Ezhil Nilavan | Assistant Professor | Paediatrics |
| 8 | Dr. Madhusudana Reddy Dasi | Assistant Professor | Paediatrics |
| 9 | Dr. Nirbheek Sharma | Assistant Professor | Paediatrics |
| 10 | Dr. Peruru Latheesh Kumar | Assistant Professor | Paediatrics |
| 11 | Dr. Karthick Sankar | Assistant Professor | Paediatrics |
| 12 | Dr. Kurvari Gourav | Assistant Professor | Paediatrics |
| 13 | Dr. Swantharia. J | Senior Resident | Paediatrics |
| 14 | Dr. Jeevitha. S | Senior Resident | Paediatrics |
| 15 | Dr. Keerthana. S | Senior Resident | Paediatrics |
| 16 | Dr. Jai Kumar. K | Senior Resident | Paediatrics |
| 17 | Dr. Aishwarya. T | Senior Resident | Paediatrics |
Department of Paediatrics
Overview
“It takes a village to raise a child” goes the saying. It takes dedicated team to treat one, bearing this in mind; our department has a fully fledged faculty and the required infrastructure to run the department seamlessly.
The Peadiatrics Department is functioning since March 2005 and has been achieving milestone after milestone.
There are 3 Pediatrics wards, NICU and PICU. All the units are well equipped with instruments and medical and paramedical staff for round the clock monitoring. In addition specialty clinics are conducted every day, to cater to children with long term illness. We constantly strive to provide quality care and ensure patient satisfaction.
Vision
- To create clinicians, competent in dealing with major health problems of children through excellence in teaching and innovative scientific research.
Mission
- To train UGs & PGs to have basic knowledge on assessment of optimal growth, development and nutrition of children and adolescents and to recognize and treat common pediatric illness.
- Provision of evidence based, high standard preventive, therapeutic and curative health services and improvement of the same through accreditations.
- To develop a centre of excellence in providing high quality intensive care for critically sick neonate and pediatric patients.
- To promote research by training and supporting academic investigators and translate these innovative approaches to optimize health outcomes in children.
Program Specific Outcomes
UG – Department of Paediatrics
Generic outcome
To acquire adequate knowledge and appropriate skills for optimally dealing with major health problems of children and to ensure their optimal growth and development.
Program Specific Outcomes (PSOs)-UG
- Ability to assess and promote optimal growth, development and nutrition of children and adolescents and identify deviations from normal
- Ability to recognize and provide emergency and routine ambulatory and first level referral unit care for neonates, infants, children and adolescents and refer as may be appropriate
- Ability to recognize children with special needs and refer appropriately
- Ability to participate in National programs related to child health and in conformation with the Integrated Management of Neonatal and Childhood Illnesses (IMNCI) strategy
- To instill professionalism by developing communication, leadership skills, ethical and moral values
- To develop lifelong learning behavior by acquiring and updating existing knowledge and skills regularly for continuous professional development
Program Specific Outcomes (PSOs)-PG
The objectives of MD Course in Paediatrics are to produce a competent pediatrician who:
- Recognizes the health needs of infants, children and adolescents and carries out professional obligations in keeping with principles of the National Health Policy and professional ethics.
- Has acquired the competencies pertaining to Paediatrics that are required to be practiced in the community and at all levels of health system.
- Has acquired skills in effectively communicating with the child, family and the community.
- Is aware of contemporary advances and developments in medical sciences as related to child health.
- Is oriented to principles of research methodology.
- Has acquired skills in educating medical and paramedical professionals.
- Ability to recognize children with special needs and to collaborate with other departments for their better outcome.
- Has developed knowledge in recognizing actually ill child and provide them emergency care.
- Ability to perform procedures as indicated for children of all ages in the primary care setting.
Program Educational Objectives(PEOs)
PEO1-Acquires competencies relevant to all aspects of Pediatrics that are essential to function as a clinical expert in providing holistic health care from newborn to adolescence for the community at all levels.
PEO2-Performs responsibilities of the provision of clinical care in keeping with the principles of National Health Policy in a professional and ethical manner
PEO3-Acquires skills in effectively communicating not only with the health team but also with the child, family, and the community
PEO4-Is oriented to principles of research methodology, enabling critical appreciation of published scientific evidence and keeping oneself up to date and disseminate scientific advances in Paediatrics and medico-legal aspects of practice
PEO5-Acquires skills and understanding of dealing with health team members, enabling system-based practice.
Faculty List
Facilities
Laboratory
Each Pediatric ward is supported by a side laboratory where basic blood, urine and stools investigations are carried out.
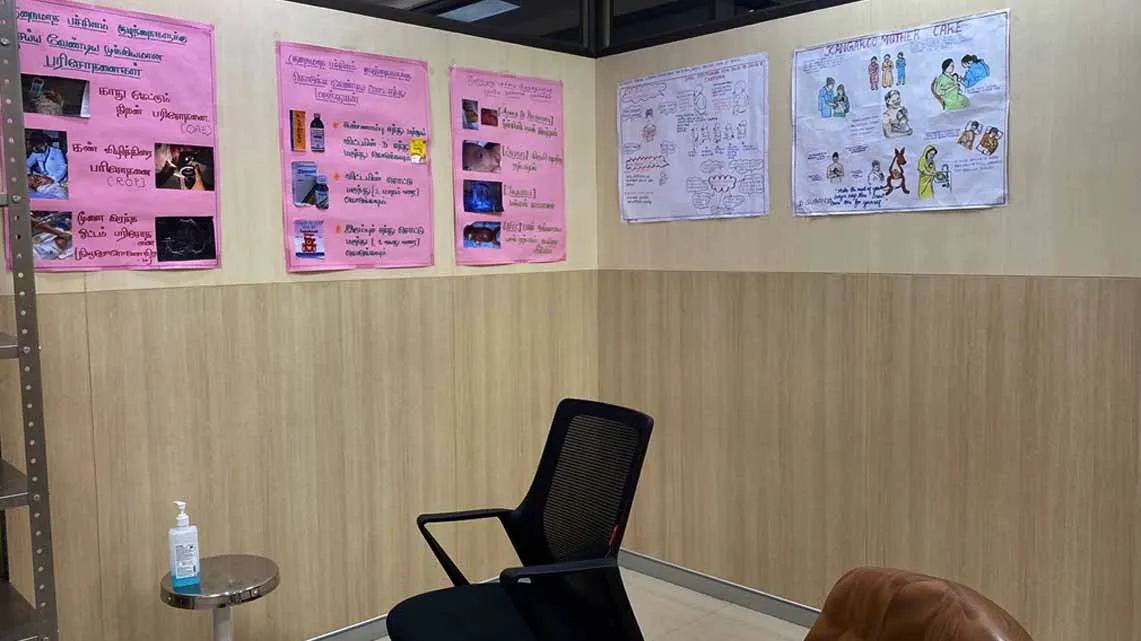
Museum
The department has got a Museum in the Clinical Department of the Hospital. Pictures depicting children with signs of important diseases, deficiencies etc. are displayed.
The Departmental Library
The Departmental Library is well equipped with 172 books on Pediatrics and related subjects. There is a Central library with varieties of books related to Pediatrics and its sub specialties. A number of Regional, National and International journals of Pediatrics are also available in the Central Library of the Medical College.
Out Patient Department (OPD)
The Out Patient Department (numbered 39) is in the ‘E’ wing of the ground Floor of the Hospital. It has adequate space for Reception and Registration of our Patients, a cubicle for special clinics, four cubicles for consultation and a separate cubicle for the admitting Unit Chief. In addition there is a treatment room, a demonstration room for Medical Students and a Record room. There is a separate breastfeeding room for nursing mothers.
The number of Out Patients attending the OPD will be in the range of 175-180 per day and around 15 children are admitted for In Patient Care every day.
Pediatric Ward
There are four Pediatric wards for four units. The I Pediatric Unit is located at the “F” wing of the III floor of the hospital capable of accommodating 30 children. The II, III and IV Pediatric Units are housed in the ‘G” wing of the III floor of the hospital, each capable of accommodating 30 child patients. Each Pediatric unit is functioning under one Professor of Pediatrics and a minimum of 2 qualified Assistant professors. On an average, 70 child patients are given inpatient treatment at any given time by the three Pediatric Units. A qualified Pediatrician is on 24 hrs duty on rotation to attend to emergencies as well as resuscitation of babies born of interventional deliveries like Caesarean section.

Pediatric Intensive Care Unit (PICU)
Very seriously ill children are looked after in a Pediatric Intensive Care ward. There are 20 such beds with all supporting facilities like Ventilators, Multipara monitors, Central oxygen supply, Central suction, CPAP machines, along with a stock of life saving drugs.
Neonatal Intensive Care Unit (NICU)
Our NICU has 20 beds and caters to both inborn and outborn neonates. It has a outborn unit, Level 2 unit and level 3 unit. There is a separate room for giving Kangaroo Mother care and breastfeeding. It is equipped with warmers, phototherapy units, ventilators, HFNC, CPAP machines and portable x-ray unit, ultrasound and 2D echo machines. High risk procedures requiring skill, such as exchange transfusions, surfactant administration, and central line insertions are being done regularly.
Both the PICU and NICU are supported by Clinical Laboratories round the clock for doing emergency investigations and Radiology department for emergency X-ray, CT and MRI.
Postnatal Ward (PNW)
There are 30 beds in postnatal ward. It is supervised and treated by our Pediatric Assistant Professors along with Postgraduates and here the newborn babies are screened for jaundice and sepsis. Screening for Congenital hypothyroidism, Sp02 screening for critical congenital heart diseases, Hearing screening using OAE is done for all neonates before discharge. Regular lactation counselling is given for all postnatal mothers by social worker.
Regular health talks are given to postnatal mothers and to their relatives adding to the comprehensive care of newborns.

Operation Theatre
Pediatric surgical problems are attended by a qualified Pediatric Surgeon of our hospital. There are facilities for Pediatric Endoscopy, Bronchoscopy etc.
Research Laboratory
A Research Laboratory has been established in the Clinical Department in the II Floor of the Hospital with adequate infrastructure.
Instruments Available
PICU
| S.No | Name of the Equipments |
|---|---|
| 1 | Paediatric Ventilator(NELCOR) |
| 2 | Multipara Monitor |
| 3 | Pulse Oximeter |
| 4 | Defibrillator |
| 5 | Syringe Pump |
| 6 | Infusion pump |
| 7 | Adult Ambu bag |
| 8 | Pediatric Ambu bag |
| 9 | Adult laryngoscope |
| 10 | Pediatric laryngoscope |
| 11 | Nebulizer |
| 12 | Central Oxygen supply |
| 13 | Vaccum suction wall mounted |
| 14 | Digital Weighing Scale |
| 15 | Newborn Weighing Scale |
| 16 | B type Oxygen cylinder |
| 17 | Pneumotic BP apparatus |
| 18 | Glucometer |
| 19 | Crash cart |
| 20 | Xray Lobby |
| 21 | Diagnostic set s- LP set |
| 22 | Cut down set |
| 23 | ICD tray |
| 24 | Electrical suction apparatus |
| 25 | ECG machine |
| 26 | Ophthalmoscope |
| 27 | Otoscope |
| 28 | HFNC |
NICU
| S.No | Name of the Equipments |
|---|---|
| 1 | Neonatal Ventilator(Maquet) |
| 2 | CPAP |
| 3 | Multi Para Monitor |
| 4 | Pulse Oximeter |
| 5 | Oxygen blender |
| 6 | T-piece Resuscitator |
| 7 | Defibrillator |
| 8 | Transcutaneous bilirubinometer |
| 9 | Radiant Warmer |
| 10 | Phototherapy unit -double |
| 11 | Phototherapy unit -single |
| 12 | Infusion pump |
| 13 | Syringe pump |
| 14 | Crash cart |
| 15 | Electrical Suction apparatus single |
| 16 | Central Oxygen supply |
| 17 | Vaccum suction wall mounted |
| 18 | Glucometer |
| 19 | Laryngoscope |
| 20 | Neonatal Ambu bag |
| 21 | Pediatrics Ambu bag |
| 22 | B type Oxygen cylinder |
| 23 | Needle destroyer |
| 24 | Digital weighing scale |
| 25 | Infant weighing scale |
| 26 | Otoscope |
| 27 | Ophthalmoscope |
| 28 | Diagnostic set s- LP set, Cut down set, Exchange tranfusion set, Dressing tray |
| 29 | Xray view box |
| 30 | Xray machine |
Special Clinics
| Day | Name of the Clinics | Time |
| Mondays | Neurology Clinic | 9.00a.m to 4.00p.m |
| Tuesdays | Well Baby clinic/Immunization Clinic | 9.00a.m to 4.00p.m |
| Tuesdays | Endocrinology Clinic-Alternate I & III | 9.00a.m to 4.00p.m |
| Tuesdays | Hematology Clinic/Thalassemia Clinic-Alternate II & IV | 9.00a.m to 4.00p.m |
| Tuesdays | Nutrition Clinic | 9.00a.m to 4.00p.m |
| Wednesdays | Pulmonology Clinic/Gastroenterology Clinic | 9.00a.m to 4.00p.m |
| Thursdays | High Risk Newborn clinic | 9.00a.m to 4.00p.m |
| Fridays | Cardiology Clinic | 9.00a.m to 4.00p.m |
| Fridays | Child Guidance clinic | 9.00a.m to 4.00p.m |
| Saturdays | Nephrology clinic | 9.00a.m to 1.00p.m |
| Daily | Diarrhoea Clinic | 9.00a.m to 4.00p.m |
Clinical Activities
Each Special Clinic is functioning under a qualified Pediatrician, supported by other Specialists wherever applicable like Dietician, Urologist, Neurologist, Psychiatrist, Psychologist, Physiotherapist etc.
A qualified Pediatrician visits the Urban and Rural Health Centers run by SMVMCH on Fridays at Thiruvennainallur.
A qualified Pediatrician in turn attends Health Camps conducted under Chief Ministers extended Health Scheme.
Academics
Undergraduate
Goals
The broad goal of the teaching of undergraduate students in Pediatrics is for them to acquire adequate knowledge and appropriate skills for optimally dealing with major health problems of children and to ensure their optimal growth and development.
Objectives-Knowledge & Skills
At the end of the course, the UG student shall be able to:
- Diagnose and appropriately treat common pediatric and neonatal illnesses.
- Describe the common pediatric disorders and emergencies in terms of epidemiology, etiopathogenesis, clinical manifestations, diagnosis, rational therapy and rehabilitation.
- Identify pediatric and neonatal illnesses and problems that require secondary and tertiary care and refer them appropriately.
- Advise and interpret relevant investigations.
- Counsel and guide patient’s parents and relatives regarding the illness, the appropriate care, the possible complications and the prognosis.
- Provide emergency cardiopulmonary resuscitation to newborns and children.
Teaching includes clinical postings, small group teaching and didactic lectures as prescribed by the NMC.
Clinical and Theory Postings
Theory Postings
The Theory postings are as scheduled as follows:
| Batch | Month | Day |
|---|---|---|
| Phase 3 Part 1 | February – July | Every Monday |
| Phase 3 Part 1 | July - December | Every Monday and Every Tuesday |
| Phase 3 Part 2 | March – July | 1st, 3rd& 5th Monday and All Saturday |
| Phase 3 Part 2 | July to November | All Fridays |
Clinical postings
The clinical postings are as scheduled as follows:
| Batch | Weeks |
|---|---|
| Phase 2 | 2 Weeks Posting + 2 weeks posting |
| Phase 3 Part 1 | 4 Weeks Posting |
| Phase 3 Part 2 | 2 Weeks Posting + 2 Weeks Posting |
Integration
The training in Pediatrics is integrated with other disciplines including Anatomy, Physiology, Biochemistry, Pathology, Pharmacology, Microbiology, ENT, Ophthalmology, Medicine, Surgery, Community Medicine, Obstetrics and Physical Medicine & Rehabilitation, to prepare the students to deliver preventive, promotive, curative and rehabilitative services for care of children both in the community and at hospital as part of a team.
Training and Learning Methods
Lectures, Small group discussions, Seminars, Tutorials, Quiz, Debates, Problem Based Learning, Videography, Integrated teachings, modular teaching and e-modules are some of the teaching methods of UG students. They are also encouraged to participate in various health programs conducted by the department.
Plan of Examination
Periodical examinations in Pediatrics Theory are conducted twice in Phase 3 Part 1 and thrice in Phase 3 Part 2. Model exam is conducted 2 months prior to their University exams.
Total of five Clinical tests are conducted, each at the end of every clinical posting, and the average is taken along with the Records marks as internal Clinical marks.
The Pass percentage of UG students in the University exam in Pediatrics department is between 90% and 95%.
Many of our students have secured gold medals in University examination every year.
Internship training (CRRI)
A two day training programme is organized for the newly joined interns in the beginning of their posting on neonatal resuscitation, common pediatrics emergencies and drug dosing in children. They are posted in NICU, PICU, Postnatal wards and general wards in order to expose them to common neonatal and pediatric problems, so as to establish confidence in managing any cases, once they go out of our college.
Postgraduates
M.d. Paediatrics Degree – 3 years of Training Program GoalsThe goals of MD course in Paediatrics are directed towards developing a competent pediatrician who:
(i) Appreciates and recognizes the health needs of infants, children and adolescents and carries out professional obligations in keeping with principles of National Health Policy and professional ethics;
(ii) Has acquired the clinical competencies pertaining to delivery of appropriate, cost effective, quality pediatric health care- preventive, promotive, curative and rehabilitative- activities that are required to be practiced in the community and at all levels of health care system;
(iii) Has acquired skills in effectively communicating with the child, family and the community;
(iv) Has acquired teaching and training skills in educating medical and paramedical professionals
(v) Appreciates the need and keeps updating the knowledge and skills pertaining to contemporary advances and developments in medical sciences as related to child health;
(vi) Has developed scientific temper and is oriented to principles of research methodology and clinical epidemiology. Objectives
At the end of the 3 year- MD course in Paediatrics, the Paediatic Trainee / student should be able to:
- Appreciate and recognize the key importance of maternal and child health in the context of the health priority of the country;
- Practice Pediatric health care delivery services in keeping with the principles of professional ethics;
- Identify social, economic, environmental, biological and emotional determinants of child and adolescent health, and institute diagnostic, therapeutic, rehabilitative, preventive and promotive measures to provide holistic care to children;
- Appreciate the importance of growth and development as the very foundation of Paediatrics and help each child realize her/his optimal growth and development potential;
- Demonstrate adequate level of proficiency and competency in basic clinical skills, e.g. taking clinical history, conducting thorough clinical physical examination including assessment of physical growth and neuro developmental and behavioural development and in arriving at the most likely or possible clinical diagnosis, in identifying precipitating or predisposing factors; high risk and low risk groups and good and bad prognostic factors;
- Plan and perform relevant, cost-effective investigative and therapeutic procedures in confirming the possible diagnosis and excluding the other differential diagnosis;159
- Develop analytical skills in the interpretation of important diagnostic, imaging and laboratory results;
- Diagnose illness in children based on the analysis of history, physical examination and investigative work up;
- Plan and deliver comprehensive treatment for illness in children using principles of rational drug therapy and Evidence Based Medical principles;
- Plan and advise measures for the prevention of childhood diseases and disabilities.
- Plan rehabilitation of children suffering from chronic illness and handicap, and those with special needs;
- Manage childhood emergencies efficiently
- Provide comprehensive care to normal, ‘at risk’ and sick neonates;
- Demonstrate skills in accurate, meaningful and concise documentation of clinical case details, and in collection of periodical and cumulative morbidity and mortality data relevant to the assigned situation;
- Develop sensitivity and appreciate the emotional and behavioural characteristics and needs of children, and keep these fundamental attributes in focus while dealing with them;
- Demonstrate empathy and humane approach towards patients and their families and respect their sensibilities;
- Demonstrate effective communication and counselling skills in explaining management options, prognosis and in providing health information and health education messages to patients, families and communities;
- Develop self learning skills as a self-directed learner and recognize the need for updating knowledge and clinical practical and technical skills pertaining to his/her professional area of practice; in selecting appropriate and accurate learning resources, and critically analyze relevant published literature in order to practice evidence-based Paediatrics;
- Demonstrate competencies in the application of basic concepts of research methodology and epidemiology in collection, interpretation and publication of scientific medical data;
- Facilitate learning of medical/nursing students, practicing physicians, paramedical health workers and other providers as a teacher-trainer;
- Play an effective and responsible role in the training and implementation of assigned National Health Programmes;
- Organize and supervise the desired managerial and leadership skills;
- Function as an effective and productive member of a team engaged in healthcare, research and education;
- Recognize the diagnostic and management limitations of the health facility and the need for appropriate and timely referral of children to higher health facilities and speciality care;
- Recognize the need for medico-legal registration and referrals of specific cases and maintenance of appropriate documentation of case details and
- Put to practice the principles of medical ethics and maintain the integrity and dignity of the chosen profession.
- Carry out resuscitation, triaging and offer appropriate medical help to affected children during disasters.
4.0 TEACHING PROGRAM
4.1. General Principles- Acquisition of practical competencies being the keystone of postgraduate medical education, postgraduate training should be skills oriented.
- Learning in postgraduate program should be essentially self-directed and primarily emanating from clinical and academic work. The formal sessions are merely meant to supplement this core effort.
In addition to bedside teaching rounds, at least 5 hours of formal teaching per week are a must. The departments may select a mix of the following sessions:
- Case presentation, case workup,
- Laboratory performance : twice a week
- Journal club : once a week
- Seminar : once a fortnight
- Case Discussions : once a fortnight/month
- Interdepartmental case or seminar : once a month
Note: These sessions may be organized and recorded as an institutional activity for all postgraduates. 4.3. Rotations
The postgraduate student should rotate through all the clinical units in the department. In addition, following special rotations should be undertaken: A. Rotational clinical / community / institutional postings
Final decision that determines “external” postings outside the primary department will differ according to department needs, feasibility, sub-speciality availability and accessibility. Apart for mandatory postings, ‘external’ postings listed below are highly recommended (desirable) to expose postgraduates to allied Pediatric sub-specialities given existing trends in practice. Specific Learning Outcomes need to be defined for each of these postings even assessed keeping in mind the Competency based curriculum and their future professional roles as Pediatricians. Rotations are listed below: Mandatory Postings
- Paediatric emergency (minimum 1 month a year)
- Neonatology (NICU) (minimum 3 months a year)
- Intensive Care (PICU) (minimum 2 months a year)
- District Residency Programme with participation in Community Outreach Child Health Programs (at least 3 months over the entire course; 3rd or 4th or 5th semester; See Section G-b below).
Desirable postings based on need, availability, accessibility, and feasibility and may be innovatively integrated into schedule of posting to optimize learning experiences.
- Sub specialities Outpatient Clinics / observing- assisting in emergency
- Clinical
- Child Psychiatry
- Pediatric Surgery
- Developmental Pediatrics
- Pediatric Nephrology
- Pediatric Hemato-oncology
- Pediatric Cardiology
- Pediatric Gastroenterology
- Pediatric Rheumatology/Immunology/Allergy
- Genetic
- Pediatric Pulmonology
- Pediatric Dermatology
- Pediatric Endocrinology
- Adolescent Health
- DOTS, PPTCT, ART center with pediatric exposure
- Microbiology diagnostic Lab
- Radiology including CT/MRI
- Forensic Medicine especially Child related
- Neuro-rehabilitation (PMR, Physiotherapy, Occupational Therapy)
- Clinical
Research
Original Articles
- Balagopal M, Thiyagarajan P, Vinayagamoorthy.V, Venkata Naveen Kumar. A study on antibiotic prescription among the hospitalized pediatric patients at a referral centre in Puducherry, India. International Journal of Contemporary Pediatrics May-June 2017; 4(3):1-6
- Balagopal Muthusamy, Vinayagamoorthy Venugopal, Sumithra .Prevalence of anemia among the hospitalized children in a rural tertiary care teaching hospital. International Journal of Contemporary Pediatrics March-April 2017;4(2):431- 437
- Thiyagarajan P, Balagopal M, Ghosh SK, Mihir Sarkar. To study the efficacy of non-invasive ventilation in severe bronchiolitis. Pediatric review; International journal of Pediatric Research Feb 2017; 4(2):108-114
- Balagopal M, Babji NSR, Vinayagamoorthy V, Venkata NK..Clinical, laboratory profile &antibiotic use in first time Wheezers in the tertiary care centre in the rural area. Pediatric review: International journal of Pediatric Research November 2016;3(11): 818-825
- Dineshkumar N, Arulkumaran A, Revathy K, Raghavendran V.D.,Clinico-Laboratory Profile of Scrub typus-An Emerging Rickettsiosis in India. Indian j Pediatr June2016;83(12):1392-1397
- Sujay Kumar E, Lakshmi Narayanan D, Arulkumaran.A, Shilpa K, Clinical Spectrum and Epidemiological profile of patients admitted to pediatric intensive care unit at Tertiary care centre in south India. J of scientific study June 2016;4(3):1-5
- Arulkumaran A, Bharathkumar T, Dineshkumar N, Anupriya R, Raghavendran V.D Clinical Profile and Outcome of Dengue Fever case in Children by Adopting Revised Who Guidelines.: A Hospital based Study .International Journal of Scientific study May 2015;3(2):174-178
- Arul Kumaran A, DineshKumar N, Bharathkumar T, Anupriya R, Raghavendran .Clinical Spectrum and Outcome of Acute Post infections Glomerulonephritis in Children: A Hospital Based Study. International Journal of Scientific Study August 2015; 3(5): 163-166
- BharathKumar T, Arulkumaran A. Clinical Profile of Children in the age group of 6 months with Lower Respiratory Tract Infection. Journal of Evaluation of Medical and Dental sciences May 2015; 4(41):7154-7172
- Arulkumaran A, Thirunavukarasu B, Earan S, Vishwanathan IS, Sukumanaran B, Morbidity and Mortality Patterns of Late Pre-terms and Their Short-term Neonatal Outcome from a Tertiary Care Hospital Puduherry Intenational Journal Sciientific Study October 2015;3(7):158-162
Case Reports
| S. No | Title of the paper | Name of the author (First/corresponding) | Department | Name of the journal | Date of Acceptance | Date of publication | ISSN number | Link of the recognition in UGC enlistment of the Journal | Name of the indexing database | Type |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Children ‘At Risk’ of Developing Specific Learning Disability in Primary Schools | Sri Lakshmi Chordia1 & Kanimozhi Thandapani1 & Arulkumaran Arunagirinathan1 | Paediatrics | The Indian Journal of Pediatrics | 19-Nov-19 | 21.12.2019 | Electronic ISSN 0973-7693 Print ISSN 0019-5456 | https://doi.org/10.1007/s12098-019-03130-z | pubmed, europepmc, research gate, studylib.net,OUCI,Semantic scholar, X-MOL | international |
| 2 | Iron deficiency anemia as a risk factor for simple febrile seizures in pediatric patients | Bharath Kumar T.1, Kanimozhi Thandapani1*, Vinod Babu S.2 | Paediatrics | International Journal of Contemporary Pediatrics | 01-May-19 | 27-06-2019 | pISSN 2349-3283 | eISSN 2349-3291 | http://dx.doi.org/10.18203/2349-3291.ijcp20192126 | International journal of contemporary pediatrics | international |
| 3 | Prevailing pattern of feeding practices and malnutrition among infant and young children | Bharath Kumar Thirunavukkarasu, Sujay Kumar Earan | Paediatrics | International Journal of Contemporary Pediatrics | 28-Feb-19 | 30-04-2019 | pISSN 2349-3283 | eISSN 2349-3291 | http://dx.doi.org/10.18203/2349-3291.ijcp20190974 | Resaerch gate,BVS, WHO, Intrnational journal of contemporary pediatrics | international |
| 4 | How safe are our children in our own homes? accidental ingestion in children: a 6 year retrospective study from a tertiary care centre | Sujay Kumar Earan, Revathi Krishnakumar*, Sivaraman Sangili, Arulkumaran Arunagirinathan, Duvvur Preethika Reddy, Uma Maheshwari R. | Paediatrics | International Journal of Contemporary Pediatrics | 11-Feb-19 | 23-02-2019 | pISSN 2349-3283 | eISSN 2349-3291 | http://dx.doi.org/10.18203/2349-3291.ijcp20190546 | Research gate, International journal of contemporary pediatrics, WHO, | international |
| 5 | Barriers to exclusive breast feeding, the missing links: a cross sectional study from Puducherry, India | Gayathri G. Nair, Arul Kumaran Arunagirinathan, Nirmal S. R, Rajesh Yadav B | Paediatrics | International Journal of Contemporary Paediatrics | 20.03.2020 | 2020 | pISSN: 2349-3283 | https://www.ijpediatrics.com/index.php/ijcp/article/download/3218/2186 | Index Copernicus , Index Medicus for South-East Asia Region (WHO), ScopeMed Journal Index Google Scholar J-Gate Directory of Science | International |
| 6 | Measuring temperature in children, conveniently and accurately: a comparative study on different modalities of thermometry | Maha Lakshmi Jagatha, Preethi Tamilarasan*, Kuppusamy Krishnamurthy | Paediatrics | International Journal of Contemporary Pediatrics | 30-Sep-21 | 2021 | pISSN 2349-3283 | https://www.ijpediatrics.com/index.php/ijcp/article/view/4502 | Index Copernicus , Index Medicus for South-East Asia Region (WHO), ScopeMed Journal Index Google Scholar J-Gate Directory of Science | International |
| 7 | Factors Precipitating Breakthrough Seizures in Childhood Epilepsy | Kanimozhi Thandapani, K. Revathi, T. Bharath Kumar | Paediatrics | journal of pediatric neurosciences | 24-Mar-21 | 11-10-2021 | ISSN 1817-1745) | https://www.pediatricneurosciences.com/preprintarticle.asp?id=327900 | EMBASE, Pubmed central, SCOPUS,Web of science | National |
| 8 | Accidental household poisoning in children: shedding light on the common agents and risk factors | Nirmal S. Rameshkumar, Preethi Tamilarasan*, Arulkumaran Arunagirinathan | Paediatrics | International Journal of Contemporary Pediatrics | 16-Aug-21 | 13-07-1905 | pISSN 2349-3283 | https://www.ijpediatrics.com/index.php/ijcp/article/view/4421 | Index Copernicus , Index Medicus for South-East Asia Region (WHO), ScopeMed Journal Index Google Scholar J-Gate Directory of Science | International |
| 9 | A quality improvement initiative to improve the quantity of expressed breast milk among mothers whose neonates were admitted in the neonatal intensive care unit | Revathi Krishnakumar1, Kanimozhi Thandapani2, Singaravelu Manikavasagam3 | Paediatrics | Sri Lanka Journal of Child Health | 18-Feb-22 | 05-Sep-22 | pISSN1391-5452 | https://sljch.sljol.info/articles/abstract/10.4038/sljch.v51i3.10239/ | Sciverse SCOPUS, DOAJ, Google scholar | International |
| 10 | Newborn care practices in rural Puducherry; a peek into the harmful practices-a cross sectional study | Sujay Kumar Earan*, Duvvur Preethika Reddy, Arulkumaran Arunagirinathan | Paediatrics | International Journal of Contemporary Pediatrics | 06.05.2023 | 12-05-2023 | pISSN 2349-3283 | eISSN 2349-3291 | https://dx.doi.org/10.18203/2349-3291.ijcp20231432 | pubmed, index copernicus, j gate, google scholar | International |
| 11 | Mobile phones and children: exposure and pattern of usage of mobile phones among children – a descriptive cross-sectional study | Duvvur Preethika Reddy, Sujay Kumar Earan*, Thambiprabagarane Kalaimani, Arulkumaran Arunagirinathan | Paediatrics | International Journal of Contemporary Pediatrics | 19.05.2023 | 26-05-2023 | pISSN 2349-3283 | eISSN 2349-3291 | https://dx.doi.org/10.18203/2349-3291.ijcp20231492 | pubmed, index copernicus, j gate, google scholar | International |
| 12 | Do children need humans or screen? Institutional-basedcross-sectional study | Rajalakshmi M1, Reenaa Mohan1, Kanimozhi T1, Karthika Devi D S1 | Paediatrics | Sri Lanka Journal of Child Health | 24.03.2023 | PISSN-1391-5452 e-ISSN 2386-110X | sciVerse scopus,IMSEAR, CABI, google scholar | international | ||
| 13 | Stress levels in parents of neonates: an underrated aspect of neonatal intensive care? | Hemakrishnasai Mallapu, Preethi Tamilarasan, Hemanth Kumar Bondada, Arulkumaran Arunagirinathan | Paediatrics | Journal of Pediatric and Neonatal Individualized Medicine | 08.07.2023 | 29.08.2023 | eISSN: 2281-0692 | https://jpnim.com/index.php/jpnim/article/view/e120211/1001 | Scopus, SJR, Google scholar | International |
Case Reports
- Arulkumaran A, Dinesh Kumar N, Anupriya R, Balaji.S. Envenomation: an uncommon cause of respiratory distress in a neonate. International Journal of contemporary Pediatrics 2015Feb;2(1):56-8
- Dineshkumar N, Arulkumaran A, Anupriya S, Balaji S.Cyclopia-holoprosencephaly sequence: a rare entity. International Journal of Contemporary Pediatrics2015 Feb;2(1):53-55
- Dineshkumar Narayanaswamy, Arulkumaran Arunagirinathan, RevathiKrishnakumar, Sivaramansangili Incontinentia Pigmenti: A rare Genoderematosis in a Male child. Journal of Clinical and Diagnostic Research, 2015 Feb; Vol-9(2):06-08.
- Dineshkumar N, Balaji S, Sivaraman S, Arulkumaran A, Raghavendran V.D, HaimMunk syndrome – a rare genodermatosis. International Journal of Scientific study2015 Feb;2(11):187-189
- Arulkumaran A,Anupriya R,Dineshkumar N, Sivaraman S.Scrub typhus pneumonia-A forgotten entity in children-case report. Intrnational Journal of Scientific Study,2015 Feb;2(1):190-192
- Dineshkumar N, Arulkumaran A, Balaji S, Anupriya R. Congenital Nasal Pyriform Aperture Stenosis: A Rare causes of Respiratory Distress in Newborn. J clinic Neonatology 2015;4:203-5
- Sivaraman S. Revathy K, Raghavendran V.D. A rare case of schizencephaly.J.Evolution Med.Dent.Sci.November 2015:4(93):15911-15912
- Revathi K, Sivaraman S, Raghavendran V.D. Neuronal Migration disorder.J.Evolution med .Dent.Sci.December 2015; 4 (102):16808-16809.
- Dinesh N,Arulkumaran.A Kimura Disease-A rare cause of Neck swelling Pediatric review, International Journal of Pediatric Research-July-September 2014; 1(2):64-67
- Balaji S, Indu SV, Dinesh N, Raghavendran VD, Spondylocostaldystosis with Sprengel Deformity. A rare association. International Journal of Pediatric Research. July-September 2014;Vol 1(2): 54-57
- Prijo Philip, Sandra Premkumar, Arulkumaran.A, Indu S, Vishwanathan, Raghavendran Sjogren-Larsson syndrome- a case report Indian Journal of Basic and applied Medical research Sep 2014; Vol 3(4):240-42
- Arulkumaran A, Balaji S, Dineshkumar N, Raghavendran VD. Abdominal Mass in a Neonate: A case of neglected posterior urethral value. Of Evolution of Med and Dent Sci 2014 Nov;3(61):13602-6
- Arulkumaran Arunagirinathan, Dineshkumar Narayanaswamy, AnupriyaRaghavan, BalajiSukumaran. A rare case of Bilateral Empyema in an Infant-Case report. Indian Journal of Neonatal Medicine and Research. 2014 Dec; Vol 3(4):1-2
- Arulkumaran Arunagirinathan, JeyakumariDuripandian,GopalRangaswamy, Smita Shivekar Prachisaban, Sunil Shivekar.Bilateral breast abscess in a neonate- A case report.IJCRI- International Journal of Case reports and Images, Vol.2,May2011;2(5)
| S. No | Title of the paper | Name of the author (First/corresponding) | Department | Name of the journal | Date of Acceptance | Date of publication | ISSN number | Link of the recognition in UGC enlistment of the Journal | Name of the indexing database | Type |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Atypical arthritis in a toddler: beware, save the heart | Sharani Boopathy, Kanimozhi Thandapani, Arulkumaran Arunagirinathan | Paediatrics | International Journal of Contemporary Paediatrics | 0l April 2020 | 2020 | pISSN: 2349-3283 | https://www.ijpediatrics.com/index.php/ijcp/article/download/3358/2246 | Index Copernicus , Index Medicus for South-East Asia Region (WHO), ScopeMed Journal Index Google Scholar J-Gate Directory of Science | International |
| 2 | Wilson disease: early screening for better living | Maha Lakshmi Jagatha, Arulkumaran Arunagirinathan, Bondada Hemnath kumar | Paediatrics | International Journal of Contemporary Paediatrics | 30-Mar-20 | 2020 | pISSN: 2349-3283 | https://www.ijpediatrics.com/index.php/ijcp/article/download/3311/2249 | Index Copernicus , Index Medicus for South-East Asia Region (WHO), ScopeMed Journal Index Google Scholar J-Gate Directory of Science | International |
| 3 | Persistent vomiting, an alarm sign in children | Ramya G, Arul Kumaran A, Tanay Gupta | Paediatrics | International Journal of Contemporary Paediatrics | 07-Apr-20 | 2020 | pISSN: 2349-3283 | https://www.ijpediatrics.com/index.php/ijcp/article/download/3345/2294 | Index Copernicus , Index Medicus for South-East Asia Region (WHO), ScopeMed Journal Index Google Scholar J-Gate Directory of Science | International |
| 4 | Generalized Bullae – A Common Drug with an Alarming Side Effect! | Anupriya Chandrasekaran1, Kanimozhi Thandapani2, Arulkumaran Arunagirinathan | Paediatrics | Annals of R.S.C.B | 05-May-21 | 2021 | ISSN: 1583-6258 | https://www.annalsofrscb.ro/index.php/journal/article/view/10139/7366 | Scopus | International |
| 5 | An uncommon organism causing necrotizing pneumonia in a toddler | Manju Reka S. B.1*, Arulkumaran Arunagirinathan1, Anupriya Chandrasekaran1, Yuvarajan S.2 | Paediatrics | International Journal of Contemporary Pediatrics | 15-Nov-21 | 2021 | pISSN 2349-3283 | eISSN 2349-3291 | https://dx.doi.org/10.18203/2349-3291.ijcp20214542 | International Journal of contemporary pediatrics,Research gate | International |
| 6 | A Rare Hemoglobinopathy Presenting as Chronic Hyperbilirubinemia | Lenaa Sakthiyavathy Manivannan, Kanimozhi Thandapani, Arulkumaran Arunagirinathan | Paediatrics | JK Science: Journal of Medical Education & Research | 15-Nov-20 | 20-Aug-21 | pISSN: 0972-1177 | https://journal.jkscience.org/index.php/JK-Science/article/view/79 | JK science, Proquest, | International |
| 7 | Diabetic ketoacidosis masquerading behind alkalemia an undiagnosed or missed variant of diabetic ketoacidosis | Vishnu Priyaa Rajasegaran*, Preethi Tamilarasan and Thambiprabagarane Kalaimani | Paediatrics | Journal of Pediatric Endocrinology and Metabolism | June 20, 2022 | July 13, 2022 | 0334018X, 21910251 | https://doi.org/10.1515/jpem-2022-0115 | Pubmed, De Gruyter,Research gate, | International |
| 8 | Post Traumatic Cerebellar Ataxia – A Least Pondered Diagnosis | Sridhar Shobana, Krishnakumar Revathi, Thirunavukkarasu Bharath Kumar | Paediatrics | Journal of Nepal Paediatric Society (JNPS) | 12.01.2023 | 31-12-2022 | ISSN 1990-7974 (print) ISSN 1990-7982 (online) | https://doi.org/10.3126/jnps.v42i2.42915 | UGC CARE, Scopus, DOAJ | International |
| 9 | Rare Clinico-radiological Syndrome Mimicking Transient Ischemic Attack | Dinesh M Sarathy1, Kanimozhi Thandapani1, Arulkumaran Arunagirinathan1, Umamageshwari Amirthalingam2 | Paediatrics | Journal of Nepal Paediatric Society (JNPS) | 15-Dec-22 | 31-12-2022 | ISSN 1990-7974 eISSN 1990-7982 | https://doi.org/10.3126/jnps.v42i2.43002 | UGC CARE, Scopus, DOAJ | International |
CME organized by the department
| S.No | Title of the CME | Period | Sponsor |
| 1. | Paediatric CME | March 2012 | IAP Villupuram, Puducherry &SMVMCH |
| 2. | National Polio surveillance update 2014 | 24th January 2014 | Indian Academy of Paediatrics |
| 3. | Recent trends in Immunization | 6th April 2015 | SMVMCH |
| 4. | Approach and management of Childhood Asthma | 26th July 2015 | SMVMCH |
| 5. | Nutricon –CME on Childhood -2016 | 25th Sep 2016 | IAP Villupuram – Puducherry &SMVMCH |
| 6 | CONPEDS’18 | 14th Oct 2018 | IAP Villupuram -Puducherry-Cuddalore Chapters jointly organised |
Workshops conducted
- Workshop on IAP Neonatal Resuscitation Programme – Golden Minute Project on 9thFebruary 2014.
- Workshop on “Neonatal Resuscitation” for Staff Nurses organized by Department of Pediatrics For on 2ndand 3rd June – 2016.
- Workshop on “Pediatric Basic Life Support and Management of common Pediatric Emergencies” for Staff Nurses on Nov 29thand 30th of 2016.
- Workshop on “Breast feeding” conducted for staff nurses along with NYCF foundation on 03rdAugust 2017.
- Workshop on “Neonatal Resuscitation for staff nurses” conducted on 20thNovember 2017.
- Workshop on “IAP-NRP FGM (BNRCP PROVIDER COURSE” for staff nurses on 12th October 2019.
- Workshop on “IAP TRAC workshop” on 10th November 2019
- Workshop on “Neonatal Resuscitation workshop (IAP NRP- FGM)” for staff nurses conducted on 27th February 2021.
- Workshop on “IAP – First Golden Minute Neonate Resuscitation conducted on 23th December 2022
Awards
- Dr.Singaravelu .M was awarded as Best Teacher award by Tamilnadu Dr.M.G.R University in the year 2012.
- Awarded as Best doctor by Tamilnadu government in the year 2013.
- Fellowship in IAP (FIAP) by National Pediatric Association.
- Best Doctor Award by IMA Tamilnadu State Board in 2015.
- A.P.J. Abdul Kalam award for social services by Thamiz IsaiMandram in the year 2017.
- Best doctor Award by IMA – Tanjore branch in the year 2018.
- Senior Pediatrician award by IAP – Tamilnadu state branch in the year 2018.
- Mamannan Raja Raja Cholan award by District administration of Tanjore in 2018.
- V.Balagopalraju Active Pediatrician award by IAPTNSC
- Arulkumaran Active Pediatrician Award by IAP – Tamilnadu State Chapter in Madurai Pedicon in the year 2022
University gold Medalist of Undergraduates in Pediatrics – Batch wise:
| Name of the Under graduates | Batch | University exam medal |
| Vaishnavi Devi.V | 2006-2011 | Gold |
| Karthika Vimal.CH | 2007-2012 | Gold |
| Balamurugan.T | 2008-2013 | Gold |
| Ramya.B | 2010-2015 | Gold |
| Divyalakshmi.C | 2011-2016 | Gold |
Postgraduate Achievements:
| S.No | Name of the PG | University Exam Medal | Batch |
|---|---|---|---|
| 1 | Dr.Preethika Reddy | Gold Medal | 2015-2019 |
| 2 | Dr.Gayathri.G.Nair | Gold Medal | 2017-2020 |
Awards
| S.No | Name of the PG | Programs | Topics | Awarded | Batch |
|---|---|---|---|---|---|
| 1 | Dr.Mohammed Neha | SIMSCON 22 | Oral Presentation | 1st Prize | 2021-2024 |
Outreach
One of the Assistant professors makes regular visits on specified days of the week to Urban Center of our Institution in Tiruvennainallur where Pediatric cases are screened and treated and sick children requiring investigations and treatment are advised admission in our hospital.
In addition Pediatrician accompanies the health camp organized by the institution every month on a Sunday where pediatric patients with various alignments like CHD, renal problems are screened and patient are admitted for further management in our hospital.
One qualified Pediatrician along with the Post graduate students goes for school health camps for screening for nutritional problems, hypertension and obesity and proper health education is advised.
Rural Breastfeeding Awareness Camp
The department of Pediatrics organized two health talks as a part of WBF celebration to antenatal and postnatal mothers. One in the Koliyanur village near Villupuram and the other in theThirubhuvanai, PHC. Faculties and postgraduates gave health promotion talk to the public.
ORS Health Camp & Health Education Talk
The department of Pediatrics along with IAP Villupuram – Puducherry Chapters jointly organized a Health camp in Kumalam Govt. Middle School, Puducherry. More than 100 children were participated and interaction made with them from IV toVII standards and ORS were distributed.
A health education talk on ORS is organized in Sacred Heart Central School in Villupuram on 29thof July 2019. Students from 5th standard to 10th standard were participated. Pamphlets were distributed to the teachers on importance of ORS during acute diarrhea.
Teenage Day Celebration – Health Education Talk
The Department of Pediatrics organized a health education talk in Bonne Nehru School, Thirukannur, Puducherry on 13th Nov 2019 for Teenage Day celebration as a part of IAP Child and Adolescent Health care week celebration. Around 200 adolescent girl students were participated. Dr. Kanimozhi.T, Dr. Revathy K – Assistant Professors of Pediatrics department of SMVMCH, gave a health talk to adolescent girls on adolescent nutrition, anemia and menstrual cycle and hygiene.
IAP Healthy Life Style Day – Health Education Talk
The department of Pediatrics organized a health talk to the adolescent boys of Bonne Nehru School, Thirukannur on 19th Nov 2019 for healthy life style day celebration as a part of IAP Child and Adolescent Health care week celebration .The problems of mobile phone addiction, Obesity, mental and health issues like anxiety and depression, substance abuse among adolescent boys was also discussed. The importance of yoga ,exercises ,sports were highlighted. Among 300 boys were participated in this event and the programme was highly appreciated.
PG Alumini
| Year | Name | Designation | Institute | E mail ID |
| 2012 to 2015 | Dr.Indu | Senior Resident | Anathapuri Hospital & Research Institute,Tirvandram | [email protected] |
| 2012 to 2015 | Dr.Prijo Philip | Pediatric Nephrology fellowship | CME Vellore | [email protected] |
| 2013 to 2016 | Dr.Anupriya.R | Junior consultant | SRISHTI Hospital Puducherry | [email protected] |
| 2013 to 2016 | Dr.Balaji.S | Junior Consultant | NICU Sooriya Hospital Chennai | [email protected] |
| 2014 to 2017 | Dr.Sivaraman.S | Fellowship in Neonatology | GKNM in Coimbatore | [email protected] |
| 2014 to 2017 | Dr.Revathy.K | Assistant Professor | SMVMCH | [email protected] |
| 2015 to 2018 | Dr.Shilpa.K | Senior Resident | Alluri Sitaramaraju Academy of Medical Science(ASRAM)’ ELURU, Andrapradesh | [email protected] |
| 2015 to 2018 | Dr.Priyaja.P | Senior Resident | Chennai Medical College in Tiruchi | [email protected] |
| 2016-2019 | Dr.Umamaheshwari | Senior resident | Trichy SRM Medical college hospital and research centre, Trichy | dr.umavijai22112gmail.com |
| Dr.Sri Lakshmi Chorida | Senior resident | Indra Gandhi govt. General Hospital and Postgraduate Institute, Pondicherry | [email protected] | |
| Dr.Nirmal SR | Private Practitioner | Dr.Thulasiraman children’s Hospital, Rasipuram | [email protected] | |
| Dr.Preethika Reddy | Senior resident | Farwaniya government hospital | [email protected] | |
| 2017-2020 | Dr.Sharani.B | Senior Resident | Mahatma Gandhi Medical College and Research Institutem Puducherry | [email protected] |
| Dr.Mahalakshmi Jagatha | Senior Resident | Kim’s Cuddles, Vishakapatnam | [email protected] | |
| Dr.Gayathri.G.Nair | Assistant professor | Sri lakshmi Narayana Medical College and Hospital, Puducherry | [email protected] | |
| Dr.Ramya.G | Private practitioner in Chennai | [email protected] | ||
| 2018-2021 | Dr.Thiyagarajan.V | Assistant professor | Aarupadi veedu medical college, Pondicherry | [email protected] |
| Dr.DineshM.S | Assistant professor | Sivagangai medical college, Sivagangai | [email protected] | |
| Dr.Mohana Priya.N | Assistant professor | Meenakshi medical college, Kanchipuram | [email protected] | |
| Dr.Anupriya.C | Consultant | Chandra Lung &Child Care Speciality Clinic | [email protected] | |
| Dr. Thambiprabagarane | Assistant professor | Sri Manakula Vinayagar Medical College & Hospital, Puducherry. | [email protected] | |
| Dr.Kamidi Kishore | Senior Resident | Konaseema Institute of Medical Sciences and Research Foundation, Andhra Pradesh | [email protected] | |
| 2019-2022 | Dr.Manju Reka S.B | Senior resident | Uthamandalam medical college, Ooty | [email protected] |
| Dr.Sivaperumal.G | Senior resident | Sri Lakshmi Narayana medical college, Pondicherry | [email protected] | |
| Dr.Hema Krishna Sai.M.S | Senior resident | Sundaram medical foundation, Chennai | [email protected] | |
| Dr.Lenaa Sakthiyavathy.M | Senior resident | Rajiv Gandhi women and child hospital, Pondicherry | [email protected] | |
| Dr.Kondra Niharika | Fellowship in Neonatalgy | Mehta's children hospital, Chennai | [email protected] | |
| Dr.Yuvasri Alias Shanthini.A | Senior resident | ACS medical college, Chennai | [email protected] | |
Testimonial from PG Alumini
- Anupriya-2013 batch Pediatric faculties have immense knowledge in guiding to handle any emergencies.
- Prijo Philip -2012 batch Has necessary infrastructure and patients which enable us to gain enough experience.
- Student friendly department and encouragement in participating workshop and conferences.
- Good training in Special Clinics